Ankylosing Spondylitis
Ankylosing Spondylitis Symptoms & Treatment Options
Ankylosing Spondylitis (AS) is a rare form of arthritis that affects 0.1% to 1.4% of the population. If left untreated, AS can cause the bones of the spine to fuse together. In fact, ankylosing means just this: to stiffen or to bend.
Likewise, patients with AS will also experience inflammation of the spine, known as spondylitis. Early warning signs of AS, for example, often include pain that radiates into the buttocks from the sacrum, pelvis, or SI joint.
Inside the body, the story is a bit more complicated. Inflammation attacks the vertebrae, spinal discs, and connective tissues of the spine: your tendons and ligaments. (Tendons connect muscles to bones; and ligaments connect vertebrae to their bony neighbors.)
Swelling in these areas causes pain and makes moving the spine very difficult. As the swelling goes down, your body tries to repair the damage as if you had suffered from an injury. Scar tissue begins to form over the enthesis (any zone where a ligament or tendon links up to a bone).
This process of scar formation, called fibrosis, can go on for quite some time. However, eventually, your body will replace the scar tissue with bone, or osseous tissue. Although the aim of this is to protect the tender tissues of your spine, the end result is the loss of a moveable joint.
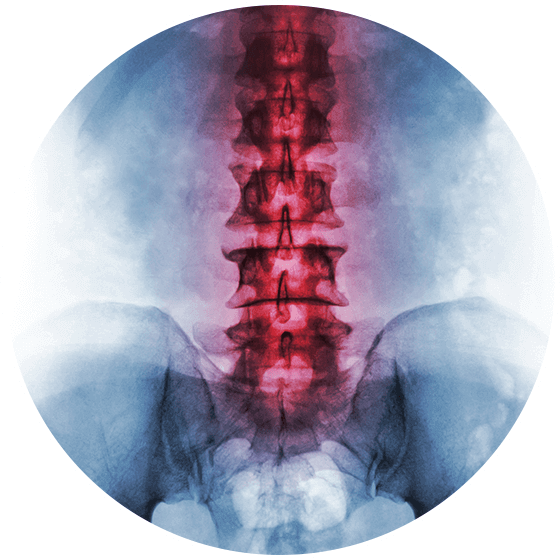
If enough vertebrae in your spine fuse together, then a patient can experience spinal rigidity, or bamboo spine. On an X-ray, your spine will appear as a singular fused column, much like a stalk of bamboo. Your doctor will no longer be able to see your spinal discs or the spaces that should exist between your bones.
If you or someone you know is experiencing AS, the following symptoms may emerge:
Pain in the cervical (neck), thoracic (mid-back), or lumbar (lower back) spine
Periodic soreness in the right then left butt cheek or vice versa
Joint pain in the hips, pelvis, SI joint, knees, or shoulders
Foot pain that affects the plantar fascia or Achilles tendon
Late night back pain or morning stiffness
Soreness that abates with movement but worsens when still
Fatigue or anemia
Flu-like symptoms, like fevers or body aches
Vomiting, nausea, or weight loss
Hardening of the cartilage in your spine, joints, breastbone, and ribs
Dactylitis, or swollen digits (like the toes)
Osteoporosis, or weak and brittle bones
Kyphosis, or forward arching of the upper back (aka hunchback)
Symptoms of Ankylosing Spondylitis
The symptoms of AS often begin gradually, with pain first arising in the right or left butt cheek. As the weeks drag on, the pain may move into the opposite side of your buttock. Because AS is rare, doctors may mistake AS for sciatica or piriformis syndrome–two very common causes of butt and back pain.
If this sounds like you, then visit a doctor whom you trust ASAP. If you try to ignore AS, then your condition will only worsen. For example, untreated AS can lead to spinal deformities (such as kyphosis), osteoporosis (or brittle bones), and osteomyelitis (or bone infections). Don’t wait to relieve your AS symptoms! Contact the arthritis and spinal deformity experts at The Advanced Spine Center today!
Who Will Develop Ankylosing Spondylitis?
85% of patients with AS have a gene known as HLA-B27. But, there is some good news. Less than 5% of people with the HLA-B27 gene will go on to develop AS. This suggests that both genetics and the environment will decide who acquires AS. Other genes that seem to play a role in AS include IL1A, ERAP1, and IL23R. However, if your doctor suspects that you have AS, then he or she will run a blood test to determine if you carry the HLA-B27 gene. (Your doctor will not test for the presence of these other genes because their role in AS is even less understood.)
Other risk factors for this condition include your age and sex. For example, men ages (17 – 45) are twice as likely as women to develop this disease, with ages 18 – 22 being the typical age of onset. Furthermore, when women do develop AS, their symptoms tend to differ from those of men. In women with AS, for example, joint stiffness often begins in the neck or hips instead of the lumbar spine.
In addition, if you have ever had ulcerative colitis, Crohn’s disease, or psoriasis, then your risk of developing AS increases significantly. (In general, these disorders tend to occur with other types of arthritis. For example, the presence of the scaly rash associated with psoriasis defines if a patient with arthritis has Psoriatic Arthritis.)
Ankylosing Spondylitis & Spinal Deformity
We cannot stress enough that AS can lead to spinal deformity. Not only will your vertebrae fuse together over time, but you are also more likely to develop osteoporosis. Osteoporosis means “porous” bones. And, excessively porous bones with low bone mineral density cannot withstand everyday forces.
Weakened vertebrae will fracture on the front side when confronted with the even slightest pressure. Even a sneeze! As more and more vertebrae shatter into this wedge shape, the spine will arc forward (aka kyphosis).
If your AS involves kyphosis, then you need a board-certified spine surgeon who specializes in spinal deformity correction, like our team of spine specialists at The Advanced Spine Center. Don’t let your life be ruled by pain and stiffness. Our doctors can help!