Posterior Cervical Laminoplasty
What is a Posterior Cervical Laminoplasty?
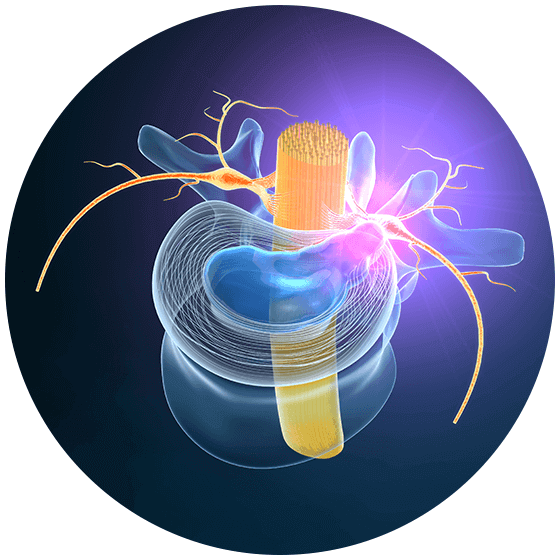
In the posterior spine, there exists a structure known as the vertebral arch. Eleven parts make up this structure—seven processes, two pedicles, and two laminae.
Sometimes, for a variety of reasons, this area of the spine becomes compressed (a condition known as cervical stenosis). This may occur because of conditions such as osteoarthritis, cervical bone spurs, disc herniations, degenerative disc disease, etc. In addition, this pressure on the cervical spine may occur at multiple levels simultaneously or at just one level. In more severe cases, this condition may lead to symptoms such as myelopathy (or spinal cord disease).
If conservative treatments do not provide the patient with adequate relief, a doctor may recommend a posterior cervical laminoplasty (PCL). A PCL relieves pressure on the spine by reconstructing the vertebral arch. This increases the space around the spinal cord and in turn, decreases any spinal cord compression.
How is a Posterior Cervical Laminoplasty (PCL) performed?
As the name indicates, a PCL accesses the spine using a small incision in the back of the neck. This is otherwise known as a posterior approach. For such an approach, the doctor will lay the patient face down on an operating table. In most cases, the performing surgeon will use special equipment to monitor the spinal cord during the operation. This method is used as a precaution to make sure that the spine remains undamaged throughout the entire process.
Unlike a laminectomy, which removes part of the lamina and other compressive structures, a PCL is more centered around reconstruction. Instead of removing the lamina outright, your surgeon will partially cut it at both ends. This effectively creates a hinge on one side of the structure, leaving a small opening at the other end. Your surgeon then opens the unhinged side, very much like opening a door. Because of this, the space around the spinal cord increases dramatically. As a natural result of this spatial increase, the pressure on adjacent spinal structures decreases. Additionally, the created space allows the spinal cord to move away from any disc herniations or bone spurs that might be compressing it further. Once this has occurred, spinal fluids will be able to move in a free-flowing path around the spine (as they should).
At this stage, the surgeon will then insert a spacer made from bone or artificial material to hold the “door” open. Incidentally, this type of minimally invasive spine surgery is also referred to as an open-door laminoplasty. In contrast, during a french-door laminoplasty, the surgeon creates two hinges on each end of the lamina and an opening through the center. However, regardless of the surgeon’s chosen method, the final outcome should be the same.
This procedure is classified as a minimally invasive surgery, so it naturally boasts the same benefits and disadvantages as similar procedures. These benefits include:
Performed on an outpatient basis or with a minimal hospital stay (case dependent)
Less scarring because of smaller incisions
Smaller incisions also translate into less trauma to surrounding tissues
Faster recovery times than open surgery
Not as painful as more invasive methods
Low risk of complication or infection
Advantages of a Posterior Cervical Laminoplasty (PCL)
Unfortunately, minimally invasive procedures are not viable in all cases. In more severe cases, for example, your doctor may need to perform a cervical disc replacement instead. However, in feasible instances where they can treat the patient’s condition, your surgeon should prefer this choice over more traditional (and painful) methods.
Aside from simply being a minimally invasive procedure, there are more specific advantages associated with receiving a PCL:
- Your surgeon will not need to remove spinal structures (like processes and pedicles)
- This procedure typically does not require spinal fusion afterward
- This is typically a less costly procedure than methods that use rods and screws
- Safer than anterior (or frontal) approaches
Anterior approaches sometimes lead to complications such as dysphagia (difficulty swallowing) or dysphonia (difficulty speaking). As PCLs are performed from the back, they are inherently safer because of it. Lastly, as there is no need for the insertion of rods and screws, PCLs are often less expensive than spinal fusion procedures.
Eligibility Requirements for a Posterior Cervical Laminoplasty (PCL)
Eligibility for any surgical procedure varies widely based on the individual. Patients with symptoms of spinal compression and myelopathy will likely need to undergo additional tests. Other extreme symptoms that may require further evaluation include tingling in the arms, balance problems, and a loss of hand movement. In many cases, specialized tests such as x-ray imaging or MRI scans are necessary to explore possible treatment routes for the procedure. X-rays will provide your doctor with images of the bones within your spine. MRI scans are a bit more detailed in that they also show the soft structures in the spine, such as discs. Furthermore, an MRI can even reveal how much pressure other structures place on the spinal cord and nerves.
Your physician will also need to obtain an extensive medical history outlining the progression of your case as well as pre-existing conditions. Note that some pre-existing conditions may increase your risk of complication or nullify your candidacy for a PCL. For more information about your specific case, consult with your doctor. He or she will give you the guidance you need, providing the best treatment options for your specific needs.
If you have a debilitating spinal condition that is not improving with time, please contact us at 973-791-4101. Our team of fellowship-trained, board-certified back specialists in NJ will ensure that your spinal stenosis treatment reflects your specific needs.